The gut microbiome—the vast ecosystem of bacteria, fungi, viruses, and other microorganisms living in the digestive tract—has moved from scientific curiosity to a central focus of modern health research. Emerging studies increasingly show that these microbes influence not only digestion, but also immune balance, metabolic health, brain function, and disease risk across the lifespan.
Rather than acting in isolation, the gut microbiome operates as a dynamic biological system shaped by diet, lifestyle, medications, and environment. Understanding how it affects long-term health is now a priority in preventive medicine and personalized care.
What the Gut Microbiome Really Does
The gut microbiome performs functions the human body cannot manage alone. These activities are foundational to long-term well-being.
Key biological roles include:
-
Breaking down complex carbohydrates and fibers
-
Producing essential metabolites such as short-chain fatty acids (SCFAs)
-
Training and regulating the immune system
-
Protecting against harmful pathogens
-
Influencing hormone and neurotransmitter production
Disruptions to this ecosystem—often called dysbiosis—are increasingly linked to chronic diseases rather than short-term digestive issues alone.
Gut Microbiome and Immune System Resilience
One of the most robust areas of research focuses on immune regulation. A healthy microbiome supports immune tolerance while maintaining the ability to respond to infections.
Recent findings suggest:
-
Reduced microbial diversity is associated with autoimmune conditions
-
Certain bacterial strains help regulate inflammatory pathways
-
Early-life microbiome composition influences immune health decades later
This connection helps explain why long-term antibiotic exposure or poor dietary patterns may increase susceptibility to inflammatory and allergic diseases.
Metabolic Health and Chronic Disease Risk
Emerging studies highlight the microbiome’s role in obesity, type 2 diabetes, and cardiovascular disease.
Microbial metabolites affect:
-
Insulin sensitivity
-
Fat storage and energy extraction from food
-
Cholesterol metabolism
People with similar diets can respond very differently depending on their gut microbiota composition, reinforcing the idea that metabolism is partly microbe-driven.
The Gut–Brain Axis and Cognitive Health
The gut and brain communicate constantly through neural, hormonal, and immune pathways—a system known as the gut–brain axis.
Emerging evidence links gut microbial balance with:
-
Mood regulation and stress response
-
Anxiety and depressive symptoms
-
Cognitive decline and neurodegenerative risk
Microbes influence the production of neurotransmitters such as serotonin and GABA, suggesting that long-term mental health may partly depend on microbial stability.
Aging, Longevity, and Microbial Diversity
Longitudinal studies show that microbiome diversity tends to decline with age, but individuals who maintain higher diversity often experience better physical and cognitive function.
Research on healthy aging indicates:
-
Diverse microbiomes are associated with lower inflammation
-
Certain bacterial profiles correlate with increased lifespan
-
Diet and lifestyle can partially reverse age-related microbial loss
These findings position the gut microbiome as a potential lever for promoting healthy longevity, not just longer life.
Diet as a Long-Term Microbiome Architect
Among all influencing factors, diet remains the most powerful and modifiable driver of microbiome composition.
Patterns consistently associated with positive microbial shifts include:
-
High intake of dietary fiber from plants
-
Fermented foods such as yogurt, kefir, and kimchi
-
Reduced consumption of ultra-processed foods
Rather than focusing on single “superfoods,” emerging research emphasizes dietary patterns sustained over years as the key to long-term microbiome health.
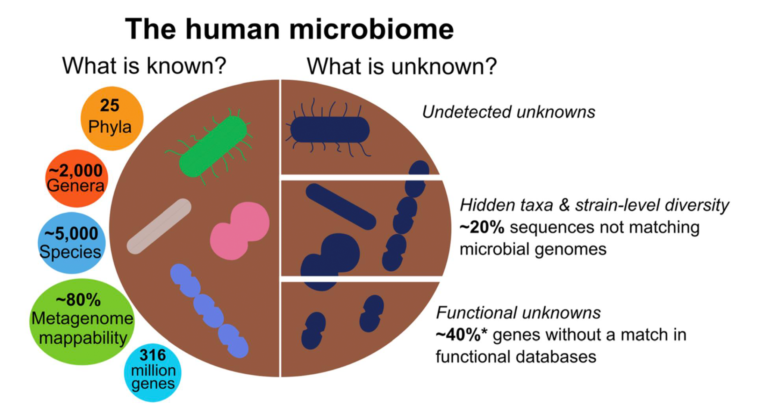
Future Directions in Microbiome Research
The next phase of microbiome science is moving toward precision and personalization.
Promising developments include:
-
Microbiome-based disease risk prediction
-
Personalized nutrition guided by microbial profiles
-
Targeted probiotics and postbiotics
-
Microbiota-modulating therapies beyond antibiotics
As methods improve, researchers aim to distinguish correlation from causation—clarifying which microbes actively drive disease prevention rather than merely reflecting health status.
Why the Gut Microbiome Matters for Long-Term Health
Taken together, emerging studies suggest the gut microbiome is not a passive passenger but an active regulator of long-term health outcomes. Its influence spans immunity, metabolism, brain function, and aging, making it a central target for future preventive strategies.
Maintaining microbial balance through consistent lifestyle choices may be one of the most practical ways to support health across decades.
Frequently Asked Questions (FAQs)
1. Can gut microbiome changes really affect health years later?
Yes. Long-term studies show that early and sustained microbiome patterns can influence immune, metabolic, and neurological health over time.
2. Is microbiome testing useful for healthy individuals?
Current tests provide insights but are best used for awareness rather than diagnosis, as clinical interpretation is still evolving.
3. Do probiotics permanently change the gut microbiome?
Most probiotics have temporary effects unless supported by long-term dietary and lifestyle changes.
4. How quickly does diet affect the gut microbiome?
Short-term changes can occur within days, but lasting benefits require consistent dietary patterns over months or years.
5. Does stress impact gut microbiome health?
Chronic stress can alter gut microbial balance through hormonal and immune pathways, affecting long-term health.
6. Are children’s microbiomes more important than adults’?
Early-life microbiome development is especially influential, shaping immune and metabolic health into adulthood.
7. Can exercise influence the gut microbiome?
Regular physical activity is associated with greater microbial diversity and beneficial metabolic effects.